Printable Do Not Resuscitate Order Template
Do Not Resuscitate Order - Customized for State
Misconceptions
Understanding a Do Not Resuscitate (DNR) Order can be challenging, and several misconceptions can lead to confusion. Here are seven common misunderstandings about DNR orders, explained for clarity.
-
A DNR means no medical care at all.
This is not true. A DNR order specifically relates to resuscitation efforts. Patients with a DNR can still receive other medical treatments and care, including pain management and comfort measures.
-
DNR orders are only for terminally ill patients.
While many people associate DNR orders with terminal illness, they can be appropriate for anyone who wishes to avoid resuscitation in the event of cardiac arrest, regardless of their overall health status.
-
Having a DNR means I will die sooner.
A DNR order does not hasten death. It is a choice about the type of medical interventions a person wants in an emergency situation. Many patients live longer, more comfortable lives with a DNR in place.
-
A DNR is permanent and cannot be changed.
This is a misconception. A DNR order can be revoked or modified at any time by the patient or their legal representative, depending on the individual's wishes.
-
DNR orders are only valid in hospitals.
DNR orders can be valid in various settings, including homes, nursing facilities, and hospice care. It is essential to ensure that the order is properly documented and communicated in each setting.
-
All healthcare providers understand my DNR wishes.
It is crucial to communicate your DNR wishes clearly with all healthcare providers. Carrying a copy of the DNR order and discussing it with family members can help ensure that your wishes are respected.
-
Only doctors can create a DNR order.
While healthcare providers typically assist in completing a DNR order, patients or their legal representatives can initiate the conversation and express their wishes regarding resuscitation.
Being informed about DNR orders is essential for making decisions that align with personal values and preferences. If there are any questions or concerns, discussing them with a healthcare professional can provide further clarity and reassurance.
Form Properties
| Fact Name | Description |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order is a legal document that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Legal Status | DNR Orders are recognized under state law, and the specific requirements for their validity can vary by state. |
| Patient Autonomy | Individuals have the right to make decisions about their medical care, including the choice to refuse resuscitation efforts. |
| State-Specific Forms | Many states have their own DNR forms, which must be completed and signed according to state regulations to be valid. |
| Governing Laws | In California, for example, the DNR Order is governed by the California Health and Safety Code Section 7180. |
| Communication | It is essential for patients to communicate their DNR wishes to family members and healthcare providers to ensure their preferences are honored. |
| Review and Revocation | DNR Orders can be reviewed and revoked at any time by the patient or their legal representative, ensuring that their wishes remain current. |
Key takeaways
Filling out a Do Not Resuscitate (DNR) Order form is an important decision that requires careful consideration. Here are some key takeaways to keep in mind:
- Understand the Purpose: A DNR order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. It is crucial to understand that this decision reflects your wishes regarding end-of-life care.
- Consult with Healthcare Providers: Before completing the DNR form, discuss your wishes with your doctor or healthcare provider. They can provide valuable insights into the implications of a DNR order and help you make an informed decision.
- Ensure Proper Documentation: After filling out the DNR form, make sure it is properly signed and dated. Keep copies in accessible locations, such as with your medical records, at home, and with your family or designated healthcare proxy.
- Review and Update Regularly: Your health status and preferences may change over time. Regularly review your DNR order to ensure it still reflects your wishes, especially after significant health changes or life events.
By keeping these points in mind, individuals can navigate the process of filling out and using a DNR order more effectively, ensuring that their healthcare preferences are respected and understood.
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, it is crucial to approach the task with care and attention. Below is a list of ten important considerations to keep in mind.
- Do ensure you understand the implications of a DNR order before completing the form.
- Do consult with your healthcare provider to discuss your wishes and any medical conditions.
- Do clearly indicate your preferences on the form to avoid any confusion.
- Do have a witness present when signing the form, if required by your state.
- Do keep a copy of the completed form in an accessible location for healthcare providers.
- Don't rush through the process; take your time to ensure accuracy.
- Don't assume that verbal instructions will be sufficient; written documentation is essential.
- Don't forget to update the form if your medical situation or preferences change.
- Don't neglect to inform family members about your DNR order and its location.
- Don't leave the form unsigned or incomplete, as this may lead to complications in emergency situations.
By following these guidelines, individuals can better navigate the process of completing a Do Not Resuscitate Order form with clarity and intent.
Common mistakes
-
Not discussing the decision with healthcare providers. It is essential to talk with doctors or medical professionals about the implications of a Do Not Resuscitate (DNR) order.
-
Failing to communicate the DNR order to family members. Family members should be aware of the individual’s wishes to avoid confusion during a medical emergency.
-
Using outdated forms. Ensure that the DNR order is current and complies with the latest state regulations.
-
Not signing the form. A DNR order must be signed by the individual or their authorized representative to be valid.
-
Neglecting to include witness signatures if required. Some states mandate that a DNR order be witnessed to be legally binding.
-
Overlooking the need for periodic review. Regularly reviewing the DNR order ensures that it still reflects the individual’s wishes and current health status.
-
Not keeping copies of the DNR order accessible. It is important to have copies readily available for medical personnel in case of an emergency.
-
Assuming that a DNR order is universally recognized. Different states may have varying laws regarding DNR orders, so it is crucial to understand local regulations.
What You Should Know About This Form
-
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that allows a person to refuse resuscitation efforts in the event of a medical emergency. This means that if a person’s heart stops beating or they stop breathing, medical personnel will not perform CPR or other life-saving measures. It is important for individuals to discuss their wishes with their healthcare providers and loved ones.
-
Who can request a DNR Order?
Typically, a DNR Order can be requested by any competent adult. This includes individuals who understand the implications of the order and can communicate their wishes clearly. In some cases, a legal guardian or a healthcare proxy may also request a DNR on behalf of someone who is unable to make decisions for themselves.
-
How do I obtain a DNR Order?
To obtain a DNR Order, you should start by discussing your wishes with your healthcare provider. They can provide you with the appropriate forms and guidance. Once the form is completed and signed by you and your physician, it becomes a part of your medical record. Make sure to keep copies for yourself and share them with family members or caregivers.
-
Is a DNR Order valid in all healthcare settings?
Yes, a DNR Order is generally valid in all healthcare settings, including hospitals, nursing homes, and at home. However, it’s crucial to ensure that the order is clearly documented and accessible to medical personnel. Some states may have specific regulations regarding the DNR process, so it’s wise to check local laws.
-
Can I change or revoke my DNR Order?
Absolutely. You have the right to change or revoke your DNR Order at any time. If you decide to do so, it’s important to communicate this change to your healthcare provider and ensure that your medical records are updated. Informing family members and caregivers is also essential to avoid any confusion in the future.
-
What should I discuss with my family about my DNR Order?
Having an open conversation with your family about your DNR Order is vital. Discuss your reasons for wanting a DNR, your values, and any specific medical situations that may arise. This ensures that your loved ones understand your wishes and can advocate for you if necessary. It can also help alleviate any potential conflicts during a crisis.
-
Are there any costs associated with a DNR Order?
In most cases, there are no direct costs associated with obtaining a DNR Order. However, some healthcare providers may charge for consultations or services related to creating the order. It’s a good idea to check with your insurance provider to understand any potential costs involved.
Do Not Resuscitate Order Example
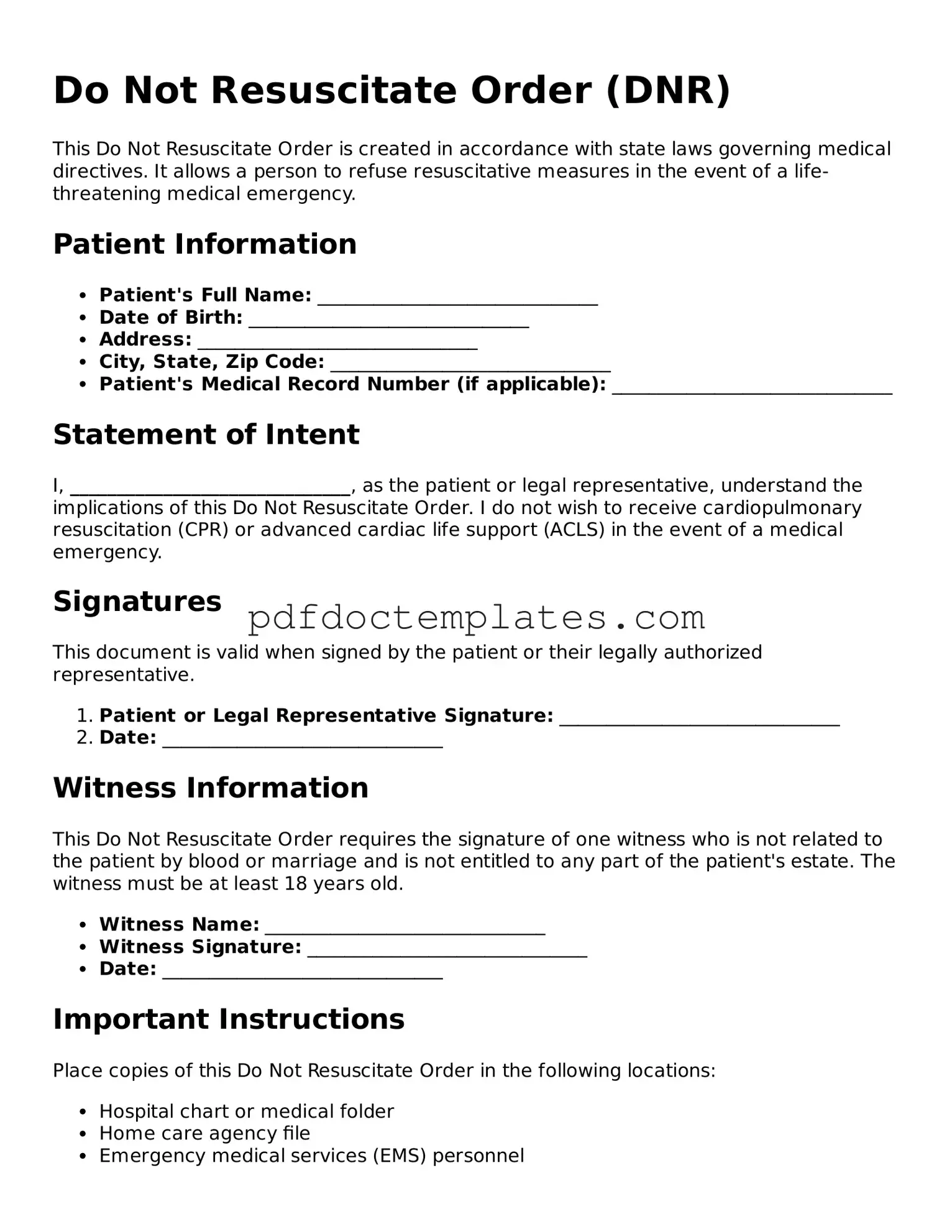
Do Not Resuscitate Order (DNR)
This Do Not Resuscitate Order is created in accordance with state laws governing medical directives. It allows a person to refuse resuscitative measures in the event of a life-threatening medical emergency.
Patient Information
- Patient's Full Name: ______________________________
- Date of Birth: ______________________________
- Address: ______________________________
- City, State, Zip Code: ______________________________
- Patient's Medical Record Number (if applicable): ______________________________
Statement of Intent
I, ______________________________, as the patient or legal representative, understand the implications of this Do Not Resuscitate Order. I do not wish to receive cardiopulmonary resuscitation (CPR) or advanced cardiac life support (ACLS) in the event of a medical emergency.
Signatures
This document is valid when signed by the patient or their legally authorized representative.
- Patient or Legal Representative Signature: ______________________________
- Date: ______________________________
Witness Information
This Do Not Resuscitate Order requires the signature of one witness who is not related to the patient by blood or marriage and is not entitled to any part of the patient's estate. The witness must be at least 18 years old.
- Witness Name: ______________________________
- Witness Signature: ______________________________
- Date: ______________________________
Important Instructions
Place copies of this Do Not Resuscitate Order in the following locations:
- Hospital chart or medical folder
- Home care agency file
- Emergency medical services (EMS) personnel
Ensure that your medical provider has a copy of this order in your medical record.
Find Other Forms
How to Gift a Car in Louisiana - Using the act of donation can provide peace of mind for both donor and recipient about property ownership.
When embarking on a homeschooling journey in California, one of the most important tasks for parents is completing the Homeschool Letter of Intent form, which serves as the official notification to the local school district regarding their intention to educate their child outside of traditional schooling.
Dd 214 - This form serves as an official record detailing a service member's military history and duty status.