Download Annual Physical Examination Template
Misconceptions
- Misconception 1: The Annual Physical Examination form is only for patients with existing health issues.
- Misconception 2: Completing the form is optional.
- Misconception 3: The form only addresses physical health.
- Misconception 4: Past medical history is not important for the current examination.
This form is designed for everyone, regardless of their current health status. Even healthy individuals should complete it to ensure comprehensive care and identify any potential health risks early.
Filling out the Annual Physical Examination form is essential. It provides healthcare providers with necessary information to deliver effective care. Incomplete forms can lead to delays or the need for additional visits.
The form covers a wide range of health aspects, including mental health, medications, and lifestyle factors. This holistic approach helps doctors understand the patient’s overall well-being and make informed recommendations.
Previous medical history is crucial. It helps healthcare providers identify patterns or recurring issues and tailor the examination and treatment accordingly. Accurate historical data can significantly impact future health outcomes.
File Details
| Fact Name | Description |
|---|---|
| Purpose | The Annual Physical Examination form collects essential health information for a comprehensive medical evaluation. |
| Patient Information | Patients must provide personal details, including name, date of birth, and address, to ensure accurate medical records. |
| Medication Disclosure | Patients are required to list current medications, their dosages, and prescribing physicians to avoid potential drug interactions. |
| Immunization Records | Documentation of immunizations, such as Tetanus and Hepatitis B, is necessary for maintaining public health standards. |
| Screening Requirements | Certain screenings, like TB tests and GYN exams, are mandated at specific intervals based on age and sex, as outlined by state health regulations. |
| Legal Compliance | In many states, the use of this form aligns with health care regulations, including those outlined in the Affordable Care Act. |
| Record Keeping | Completing the form accurately helps ensure continuity of care and supports any necessary follow-up medical evaluations. |
Key takeaways
Completing the Annual Physical Examination form is crucial for your health and well-being. Here are key takeaways to keep in mind:
- Fill Out Completely: Ensure all sections are filled out accurately to avoid delays or return visits.
- Medical History: Provide a detailed summary of your medical history, including any chronic health problems.
- Current Medications: List all medications, including dosage and prescribing physician. If necessary, use an additional page.
- Allergies: Clearly state any allergies or sensitivities to medications or other substances.
- Immunizations: Update your immunization records, noting the dates and types of vaccines received.
- Screening Tests: Include any relevant screening tests, such as TB tests, mammograms, or prostate exams, and their results.
- Hospitalizations: Document any past hospitalizations or surgical procedures with dates and reasons.
- Physical Examination: Provide accurate readings for blood pressure, pulse, and other vital signs.
- Follow-Up: Pay attention to recommendations for follow-up care, including specialist evaluations and lifestyle changes.
Taking the time to complete this form thoroughly can lead to better health outcomes. Make sure to bring it to your appointment and keep a copy for your records.
Dos and Don'ts
When filling out the Annual Physical Examination form, consider the following guidelines:
- Provide accurate personal information, including your name, date of birth, and address.
- List all current medications, including dosage and frequency, even if they seem minor.
- Be honest about your medical history and any significant health conditions.
- Indicate any allergies or sensitivities clearly to avoid potential complications.
- Check the box for communicable diseases honestly, as this is crucial for public health.
- Review the form for completeness before submission to prevent delays in care.
- Ask for assistance if you do not understand any part of the form or need clarification.
Conversely, avoid the following mistakes:
- Do not leave any sections blank; incomplete forms may require additional visits.
- Avoid exaggerating or downplaying your health issues; accuracy is essential.
- Do not forget to mention past hospitalizations or surgeries, as this information is vital.
- Refrain from using medical jargon; clear language helps your healthcare provider.
- Do not skip the immunization section; it is important for your overall health assessment.
- Do not rush through the form; take your time to ensure all information is correct.
- Avoid assuming your doctor remembers your medical history; always provide it again.
Common mistakes
-
Incomplete Personal Information: Many people forget to fill out all required fields, such as their full name, date of birth, or Social Security Number. Missing this information can lead to delays in processing and may require additional visits.
-
Neglecting Medication Details: It's common for individuals to overlook listing current medications or to provide incomplete information about dosages and prescribing physicians. This can result in potential health risks or complications during the examination.
-
Omitting Medical History: Failing to include a thorough medical history or significant health conditions can hinder the physician's ability to provide appropriate care. This includes not mentioning allergies or past surgeries.
-
Ignoring Immunization Records: Some individuals do not accurately report their immunization history. This can affect the assessment of their health status and lead to unnecessary vaccinations or tests.
What You Should Know About This Form
-
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect essential health information prior to a medical appointment. It helps healthcare providers assess a patient's medical history, current medications, allergies, and any significant health conditions. This information allows for a more efficient and effective examination, reducing the need for follow-up visits.
-
What information is required in Part One of the form?
Part One requires personal details such as name, date of birth, and address. It also asks for the Social Security Number (SSN) and the name of an accompanying person. Additionally, patients must provide a summary of their medical history, current medications, allergies, immunizations, and any previous hospitalizations or surgical procedures.
-
How should current medications be documented?
Current medications should be listed by name, dosage, frequency, diagnosis, and prescribing physician. If necessary, a second page can be attached to ensure all medications are accurately documented. It is crucial to indicate whether the individual takes medications independently.
-
What immunizations are included in the form?
The form includes sections for various immunizations, such as Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax. Dates of administration and types of vaccines received should be recorded. This information is vital for assessing the individual's immunity and overall health status.
-
What is the significance of the tuberculosis (TB) screening section?
The TB screening section is important for identifying potential exposure to tuberculosis. It requires documentation of the date the test was given, the date it was read, and the results. If the test is positive, a follow-up chest x-ray is recommended. This helps prevent the spread of communicable diseases.
-
What types of evaluations are included in Part Two of the form?
Part Two includes a general physical examination where vital signs such as blood pressure, pulse, and temperature are recorded. It also assesses various body systems, including eyes, ears, lungs, and cardiovascular health. Any abnormal findings should be noted, along with recommendations for further evaluation if needed.
-
What should be done if there are changes in health status from the previous year?
If there are any changes in health status, it is essential to specify these on the form. This information helps healthcare providers tailor their recommendations and treatment plans. Patients should also disclose any new medications or treatments that may have been initiated since the last examination.
Annual Physical Examination Example
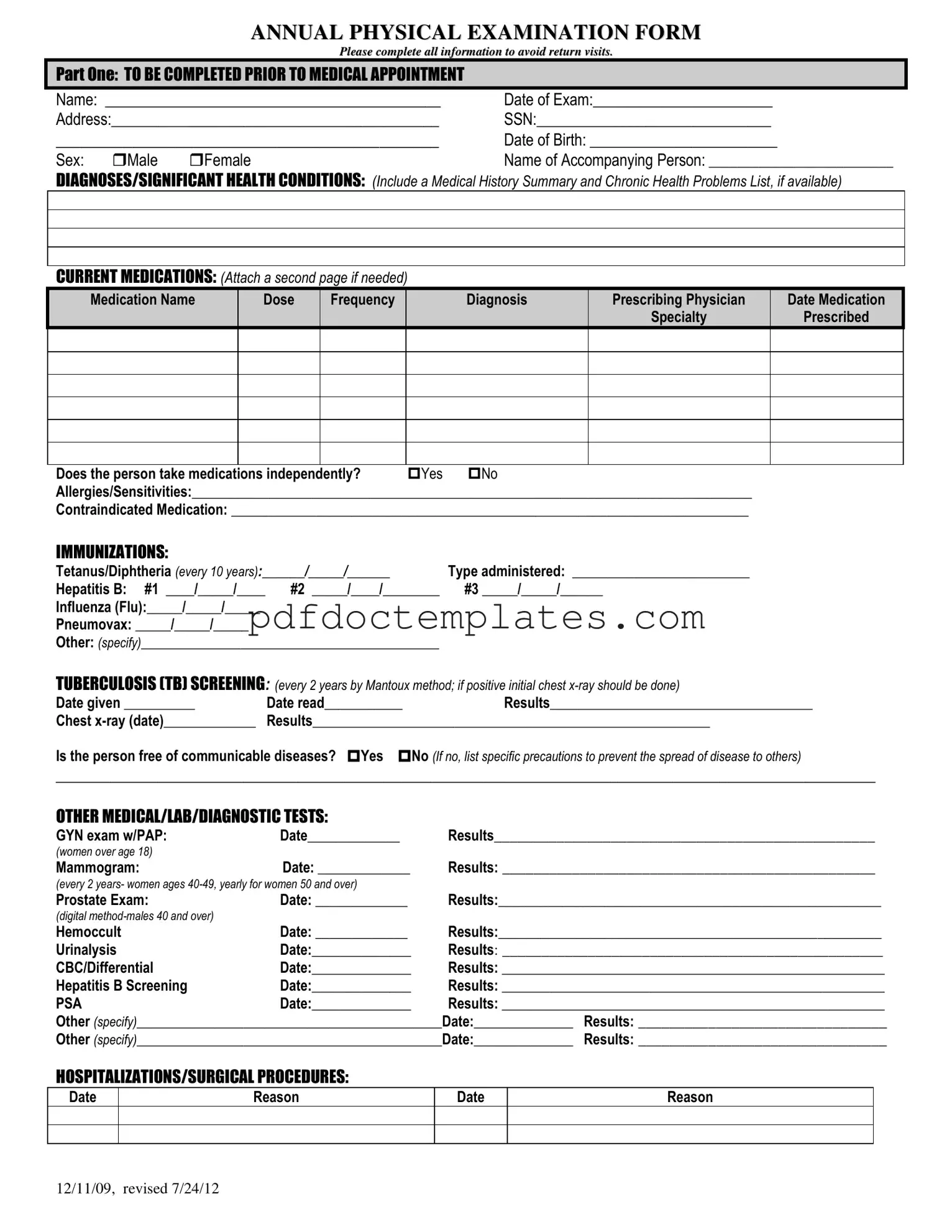
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Consider More Forms
Hazmat Bill of Lading Pdf - Halt of transportation due to shipper requests is covered in the terms.
The Florida Power of Attorney for a Child form provides a vital mechanism for parents seeking to ensure their children's well-being during times they are unable to be present. This legal document permits another trusted adult to make decisions on behalf of the child, thereby safeguarding their needs and interests. For additional resources and templates related to this important form, you can visit All Florida Forms.
Proof of Pregnancy Form Planned Parenthood California - This document emphasizes the importance of understanding all aspects of reproductive health service options.